For centuries, the fields of human medicine, veterinary science, and environmental conservation largely operated in silos. We treated human ailments, cared for our pets and livestock, and studied ecosystems as distinct entities. However, the 21st century has brought a stark realization: this fragmented approach is no longer sustainable. We are witnessing the undeniable rise of the ‘One Health’ approach – a paradigm that recognizes the profound interconnectedness of human, animal, and environmental health. This isn’t just a trendy concept; it’s an urgent necessity for a sustainable and healthy future for all.
What Exactly is One Health?
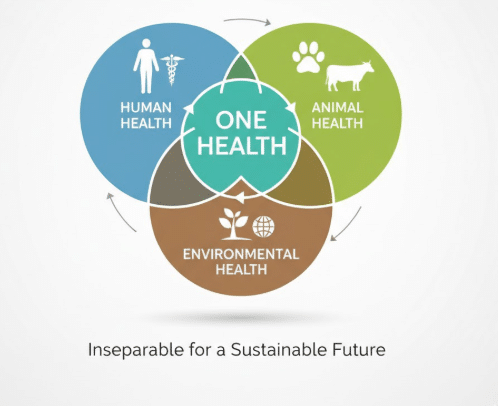
At its core, One Health is a collaborative, multisectoral, and transdisciplinary approach working at local, national, and global levels to achieve optimal health outcomes recognizing the interconnections between people, animals, plants, and their shared environment. It’s about breaking down traditional barriers and fostering communication, cooperation, and coordination among experts from diverse fields. Think of it as a holistic lens through which we view health challenges.
The Driving Forces Behind One Health’s Emergence
Several critical factors have accelerated the adoption and urgency of the One Health framework:
- Zoonotic Diseases on the Rise: A significant majority of emerging infectious diseases (EIDs) in humans – an estimated 75% – are zoonotic, meaning they originate in animals and spill over into human populations. COVID-19, SARS, MERS, Ebola, Zika, Avian Influenza, and Swine Flu are just a few stark reminders of this reality. These pathogens don’t respect species boundaries, highlighting the critical need for integrated surveillance and response.
- Antimicrobial Resistance (AMR): The overuse and misuse of antibiotics in both human and animal agriculture contribute significantly to the global crisis of antimicrobial resistance. Bacteria become resistant, making infections harder to treat, leading to prolonged illness, disability, and death. AMR is a classic One Health challenge, demanding coordinated strategies across all sectors to preserve the efficacy of these life-saving drugs.
- Food Safety and Security: Our global food systems are complex. The health of livestock directly impacts food safety and availability. Contaminants, pathogens, and residues can move from farm to fork, affecting human health. A One Health perspective ensures safer food production, better disease management in food animals, and ultimately, greater food security for a growing global population.
- Environmental Degradation and Climate Change: Deforestation, habitat loss, pollution, and climate change are altering ecosystems, forcing wildlife into closer contact with humans and domestic animals. This increased interface creates more opportunities for pathogen spillover. Climate change also influences vector-borne diseases, expanding the geographical range of disease carriers like mosquitoes and ticks. Healthy ecosystems are fundamental to healthy populations.
- The Human-Animal Bond: Beyond diseases, the deep bond between humans and animals brings significant health benefits, from improved mental health to increased physical activity. However, it also presents public health considerations, such as the spread of parasites or allergies. Understanding this bond from a One Health perspective allows for the maximization of benefits while mitigating risks.
The Tangible Benefits: A Collaborative Future
Embracing One Health isn’t just about mitigating risks; it’s about creating a more robust and resilient future.
- Early Detection and Prevention: By integrating surveillance data from human health, animal health, and environmental monitoring, we can identify emerging threats earlier, allowing for quicker intervention and prevention strategies.
- More Effective Control of Zoonoses: Coordinated efforts mean better outbreak investigation, more targeted vaccination campaigns (where applicable), and more effective public health messaging.
- Smarter Use of Resources: Breaking down silos reduces duplication of effort, fosters shared resources, and optimizes funding for health initiatives.
- Enhanced Research and Innovation: Interdisciplinary teams can tackle complex health challenges from multiple angles, leading to more comprehensive solutions and groundbreaking discoveries.
- Improved Policy Making: Policies informed by a One Health perspective are more holistic, effective, and sustainable, addressing the root causes of health issues rather than just the symptoms.
Illustrating the Impact: Data on Zoonotic Diseases
To underscore the prevalence and impact of zoonotic diseases, consider the following data:
| Disease | Primary Animal Host(s) | Human Impact (Examples) |
| COVID-19 | Bats (likely via intermediate host) | Global pandemic, severe respiratory illness |
| Rabies | Dogs, bats, wild carnivores | Fatal neurological disease |
| Avian Influenza (H5N1) | Poultry, wild birds | Severe respiratory illness, high mortality |
| Lyme Disease | Ticks (from deer, rodents) | Chronic joint pain, neurological issues |
| Ebola | Bats, non-human primates | Severe hemorrhagic fever, high mortality |
| Salmonellosis | Poultry, cattle, reptiles | Gastrointestinal illness, severe in some cases |
| Zika Virus | Mosquitoes (from primates) | Microcephaly in newborns, neurological disorders |
This table represents a small selection of prominent zoonotic diseases and their known animal origins/vectors.
Moving Forward: A Call for Integration
The One Health approach demands a fundamental shift in mindset. It requires:
- Education and Training: Integrating One Health principles into medical, veterinary, and environmental curricula.
- Policy and Governance: Developing frameworks that support intersectoral collaboration at all levels of government.
- Investment: Allocating resources to support integrated surveillance, research, and intervention programs.
- Public Awareness: Educating communities about the shared risks and responsibilities for health.
The future of health is undeniably shared. By recognizing the intricate dance between humans, animals, and our environment, and by working together across disciplines, we can build a healthier, safer, and more sustainable world for generations to come. The rise of One Health is not just a trend; it’s a vital evolution in our understanding and approach to global well-being.
Important FAQs on the ‘One Health’ Approach
Q1: Is One Health just about preventing pandemics?
A1: While preventing and responding to zoonotic pandemics is a critical component, One Health is much broader. It encompasses food safety and security, antimicrobial resistance, environmental health, chronic diseases influenced by environmental factors, mental health (e.g., impact of pet ownership), and much more.
Q2: Who is involved in a One Health initiative?
A2: A diverse range of professionals! This includes medical doctors, veterinarians, public health professionals, epidemiologists, ecologists, environmental scientists, toxicologists, microbiologists, sociologists, economists, policymakers, and more. The key is their willingness to collaborate across disciplines.
Q3: How does climate change fit into One Health?
A3: Climate change is a major driver of health issues addressed by One Health. It alters ecosystems, shifts disease vector ranges (like mosquitoes), impacts food and water security, and can lead to displacement and increased human-animal contact, all of which create new health risks.
Q4: What’s the biggest challenge for implementing One Health?
A4: One of the biggest challenges is breaking down institutional and disciplinary silos. This requires fostering communication, trust, and shared understanding among professionals who have traditionally worked independently, as well as securing sustained funding and political will for integrated programs.
Q5: Can I practice One Health in my daily life?
A5: Absolutely! Simple actions like practicing responsible pet ownership (vaccinations, hygiene), safe food handling, advocating for environmental protection, supporting sustainable agriculture, and being aware of local wildlife interactions contribute to the One Health ideal.

